Human Health
The Total Fertility Rate of the State is 3.4 a little high above the national level of 2.9. The IMR for the state has come down currently to 57 from previous figure of 95 at the time of formation of the state. This is a major achievement for the state considering the fact that any reduction in IMR requires synergistic efforts from several departments and improvement in social status. The Maternal Mortality Ratio of 335 is slightly higher than the National average. The Sex Ratio in the State is 989 a favourable one, compared to 933 for the country.
Over the last ten years the State has taken several strides to improve the delivery of health services and has been able to achieve some progress in bringing down its adverse health indicators. Sectoral allocation for Public health currently stands at 5 percent of Plan Expenditure and 0.7 percent of the NSDP. There is much scope for increasing the outlay on health in the 12th Plan, as also recommended by Planning Commission’s Approach Paper.
Health Infrastructure
The overall health infrastructure of the state has been quite poor when the state received its own independent status. Until recently, there was only one medical college for modern medicine in the state at Raipur. Similarly, the number of sub centres, primary health centres or community health centres were way below the requirement, keeping in mind that the state was sparsely populated with very remote and difficult to reach terrain with almost half of its land covered with dense forests. In the past attention was focused on improvement of health infrastructure to increase coverage and to subsequently make a dent on these indicators. As a result, facilities have seen a quantum increase in numbers from six District Hospitals to 16, Community Health Centre (CHCs) from 114 to 148, Primary Heath Centre (PHC) from 512 to 757 and Sub-Health Centre from 3818 to 5112 in the past decade. Additionally, the number of approved Anganwadi Centres (AWCs) has increased from 20,289 in 2001 to 43,763, and mini-AWCs from 836 in 2001 to 6,548 by 2011, mainly for reaching the remote and dispersed populations. Integrated Child Development Services (ICDS) beneficiaries have also doubled in this period. During Eleventh Plan period alone 9000 new AWCs and 4200 mini-AWCs have been constructed so far. The state is also having presence of large number of indigenous practitioners in the form of Ayurveda, Unani, Siddha, and other systems along with Homoeopathy.
Priorities
Several State-sponsored schemes have been launched for children, women and adolescents like CM Kanyadaan Yojana, Mitanin programme on health extension and awareness, Ayushmati, CM Bal Sandharbh Yojana and nutrition surveillance programme. The local food model for supplementary nutrition under ICDS has helped reduce malnutrition and will be further strengthened. Efforts to improve nutritional security of the most vulnerable have improved access to food grains, iodised salt, and pulses under CM Khadyaan Sahayata and Amrit Vitran schemes and will be continued
The Annual Health Survey begun since last year by the Office of Registrar General will help the state to closely tracking the health outcomes and focus attention on deserving areas- both curative and preventive. The State will strive to ensure a better convergence between sub-sectors that impact health and ensure coordinated working of institutions providing drinking water, health, nutrition, and sanitation for better achievement of outcomes.
- Strengthen capacities of health cadres to provide quality services, particularly for women and children
- Improved coverage of routine immunization & institutional deliveries
- Convergence of related-schemes for better health impact
- Universal health insurance for all vulnerable groups
- Reduce mortality and morbidity among women and children
- Enabling environment for retention, better performance and local accountability of health staff
- Revival and promotion of traditional health practices
The State had developed its own health targets that were more ambitious that the Millennium Development Goals. These were to reduce malnutrition by 33 percent, IMR by 66 percent and MMR by 75 percent, but Chhattisgarh still has a long way to go. While the achievement is significant, challenges remain high in terms of further reducing under-five malnutrition, anaemia among children of 6-36 months age group and importantly addressing the gender gap in health status on priority.
A major challenge posed to the state is the need to arrest severe and acute malnutrition grappling more than half its children. Limited ante and post-natal care, poor feeding practices among pregnant/ nursing mothers and among children, lack of adequate sanitation are among the reasons for this high level of malnourishment. About 45 percent children under 3 years of age are stunted and nearly 18 percent are wasted. As per NFHS-3, only 55 percent women in the state received the mandatory three ANC check-ups and only 25 percent received post-natal care within 2 days of delivery. While exclusive breastfeeding is practiced by more than 82 percent of the nursing mothers, colostrum is being fed by only one-fourth of the nursing mothers. The rural sanitation coverage in the state is only 57.26 percent, one of the worst amongst major states-after Bihar and Jharkhand.
The biggest bottleneck is the placement and retention of medical practitioners. Additional incentives are required for retention of senior health personnel, especially those serving in LWE areas. Current ownership of health services by PRIs is weak, as a result of which local accountability of health services is poor. Functionaries report to their line department and PRIs having little role in monitoring services. Though Panchayat Health Committees are supposed to perform this oversight, at present it is more in terms of tracking financial progress and quantitative indicators and less with quality. The primary reason for this is lack of institutional linkage with health services, something that has also been flagged in 12th Plan Approach Paper.
The State has been undertaking extensive initiatives in the health sector. Some of these are outlined below.
Governance Reforms: Empowerment of Panchayati Raj Institutions and improved efficiency of health systems are two cornerstones of National Rural Health Mission (NRHM). The mission document envisages setting up a platform for involving the Panchayati Raj institutions and community in the management of primary health programmes and infrastructure; train and enhance capacity of PRIs to own, control, and manage public health services. Further, it counsels to strengthen existing PHCs through better staffing and human resource development policy, clear quality standards, better community support and an untied fund to enable the local management committee to achieve these standards. Integrating vertical Health and Family Welfare programmes at State, District, and Block levels is another dimension of this mission. Chhattisgarh initiated several reforms in view of the above objectives. Some of the important ones are briefly described below.
- One of the key efforts of the state is appointment of a Health Commissioner at state level. The Commissioner will supervise and coordinate the activities of three state level Directors, viz. Directors of Family Welfare, Health Services and Health Training;
- Devolution of Powers to Block Medical Officers -- This is a bold step taken by the State. The Block Medical Officers have been given the power of Drawing and Disbursal Officer. Through this measure, more decentralized decisions making on health activities and quick fund release and utilization have been materialized. This effort will bear fruits after sometime and then it is likely to be held as key step in decentralised planning and implementation process; and
- Integrated Health Equipment Management System -- Health sector is mainly a service sector with 60 – 65 % of the cost going for remuneration. However, 25 – 30 % of the cost is spent on drugs and equipment. Therefore, this area offers an opportunity to undertake measures for cost containment. Keeping this in mind, the Chhattisgarh Health Equipment Management System has been created as a part of an integrated inventory management system. There are one State Cell and two regional workshops under this system. This system is taking care of rationalized procurement, immediate repair of small equipment, supervising the annual maintenance contract for costly equipment. Moreover, this system is undertaking capacity building measures to improve the skills and knowledge of different cadres of technicians in preventive maintenance and repair.
No detailed studies are currently available documenting climate vulnerability and risk to the health sector in Chhattisgarh. However, a range of other studies has shown that climate change is bound to affect the basic requirements for maintaining health. It leads to extremes and violent weather events; resurgence of disease organisms and vectors; affects the quantity of air, agriculture and water; and the stability of the ecosystems.
The current burden of disease due to climate sensitive health outcomes is considerable. Direct impacts of climate change on human health could include exposure to thermal extremes – leading to morbidity and mortality due to thermal extreme such as cardiovascular and respiratory diseases; and altered frequency and/or intensity of other weather events – leading to injuries, psychological stress; damage to public health infrastructure, by floods and other natural calamities.
Indirect impacts of climate change on human health could include effects on range and activity of infective vectors and parasites – leading to changes in geographic areas and incidence of vector borne diseases e.g. malaria, dengue fever and several types of encephalitis; altered local ecology of water borne and food borne ineffective agents because of higher temperatures – leading to changed incidence of diarrhoeal and other infectious diseases. Cholera and higher ambient temperatures foster the growth of pathogens that thrive in or on food e.g. Salmonella infection. Other impacts could include altered food (especially crop) productivity due to changes in climate and extreme weather events, and associated pests and diseases – leading to malnutrition and hunger, and consequent impairment of child growth and development. Climate change can also potentially impact the levels and biological impacts of air pollution, including pollen and spores – leading to asthma and allergic disorders, other chronic respiratory disorders and deaths. Likewise, climate change could impacts freshwater availability fresh water, in turn leading to lack of hygiene and thus increase water born diseases. They can also compound the ever-increasing traffic and exhaust as well as industrial emissions are raising concentrations of SO2, NOx, and O3 – leading to health hazards. Thermal stress – heat and cold waves are also another potential impact of climate change in human health, as are indirect impacts arising out of other climate related disasters such as floods and droughts.
The State Health Department is committed to the health and well being of all citizens and visitors to the State, and as such, the Department will take the necessary steps to gear up for the potential health impacts from climate change, while continuing to contribute to the achievement of the State’s health targets as well as the national health targets plan for 2012 – 2017.
As the highest priority agenda, a Climate Change Cell will be constituted in the Health Department, as well as district level sub-cells, and these will be mandated the task of coordinating all climate related activities of the Department under the CSAPCC as well as liaising with the State institutional and coordination mechanisms outlined in an earlier section of this report. The Department will undertake collation and review of all available material and evidence related to climate change impacts on human health, and also undertake a review of health policies, plans, and institutional frameworks in the State with a view to incorporating climate concerns.
In line with the overarching principle of improving scientific knowledge, evidence base and understanding of climate change and its impacts on human health, the Health Department will begin building a strong evidence base including collecting, compiling, and analysing relevant data and information in terms of perceptions of affected people and communities. Based on the results of the comprehensive vulnerability analyses to be undertaken by the State, will review the adequateness of its current plans and institutional frameworks to respond to climate concerns in the health sector at all levels. Plans at all levels including the District health Plans will be suitably amended.
Based on current evidence, it is anticipated that the Department will initiate action relating to:
- Undertaking measures to manage increased vector borne and water borne disease burden;
- Design and deploy improved approaches to deal with heat and wave conditions;
- Dealing with the physical and psychological impacts post-extreme weather events.
- Addressing drought, malnutrition, and food security issues; and
- Addressing food safety arising due to increased ambient temperature and extreme events.
Towards building adaptive resilience and reducing vulnerability across communities and sectors, the Department will initiate mechanisms to build adaptive capacities both within the Department and potentially, among the citizens by:
- Undertaking reviews of the State’s health infrastructure and potential climate change related vulnerabilities and risks (and where such infrastructure is found to be at high risk, retrofit to make these more climate resilient);
The Department will initiate a range of capacity building measures including:
- Awareness of people about health hazard from climatic change, covering all areas like rain water harvesting, energy efficiency, health hazards, water conservation, protection from extreme climate etc.;
- Information, education and communication efforts;
- Behavioural change communications interventions in relation to the impacts of climate change;
- Trainings and Sensitizations for Department personnel;
- Capacity Building of the all medical personnel of in districts including frontline functionaries and personnel associated with various programmes such as the Integrated Disease Surveillance Programme (IDSP), ANM, AWC, ASHA & all the medical NGO’s in the district to identify the early signs of extreme climatic effects on the population; and
- Developing and strengthening of disaster management teams in every district hospital specifically to respond to the effect of extreme climate changes.
 AIIMS,Raipur
AIIMS,Raipur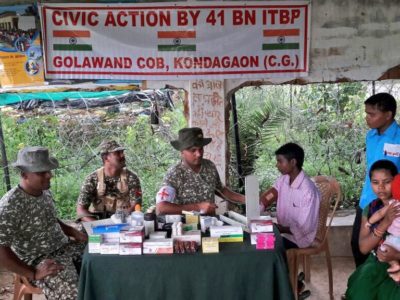 Health Camp,Kondagaon
Health Camp,Kondagaon Chhattisgarh Ambulance Service
Chhattisgarh Ambulance Service Health Checkup
Health Checkup
